Lung-protective ventilation for every patient
At Ventilation Symposium in Copenhagen, we gathered several prominent experts to speak on the subject lung-protective ventilation. Now we are making the recordings of the talks available to everyone.
Mechanical ventilation is not a new concept, but one that has evolved drastically over time: From negative-pressure ventilation to positive-pressure ventilation, from invasive to non-invasive, from constant volume and pressure to adaptive ventilation.
In the recent decades the development of ventilation technology only seems to accelerate as more new, improved ventilation modes appear. However, it also seems that shifting from using a standardized approach to an individualized approach to ventilation is still a debate. Therefore, we have written this article to provide an overview and highlight the benefits of individualized ventilation vs standardized ventilation.
Ventilators most often have different modes and a variety of settings. When we refer to standardized ventilation, we mean using the starting point, the default settings, for all patients.
Using the standard settings for ventilation is common practice, e.g., for patients that are ventilated after surgery for 3-4 hours. Individualized ventilation is more commonly used in the intensive care unit (ICU), where patients typically stay for days.
If the wrong ventilator settings are applied, e.g., if the standard mode does not fit the patient, it can damage the lungs and result in VILI. VILI (ventilator-induced lung injury) is acute lung injury caused by mechanical ventilation. Research especially refer to high tidal volumes as a cause of VILI. In other regards, studies also point to lower tidal volumes as favorable: A study has, e.g., shown that in patients with acute lung injury and acute respiratory distress syndrome (ARDS), mechanical ventilation with a lower tidal volume than what is traditionally used resulted in decreased mortality and increased the number of days without ventilator use. Even within the last ten years studies suggest driving pressure should be lower than 15 cm H2O, which has led to further investigation of the influence of mechanical power on mortality.
Overall, it can be said that being connected to a ventilator is unnatural. The longer a patient is ventilated, the more likely it is that complications occur, because there is an increased risk is of catching infections like pneumonia or other infections. This may increase the length of the patient’s stay in the hospital and consequently the costs. To reduce the damage of the ventilation and the risk of complications, individualized ventilation can be utilized.
As the name indicates, individualized ventilation is ventilation that is adapted to the individual patient. An individual approach is applied because all people and all lungs are different. Even on different days, the same patient also needs different ventilation strategies for the optimal care.
Tina Harboe Otte, Nordic Business Unit Manager, says: “When we talk about lung-protective ventilation, this to a large extent means ventilation adapted to the individual. Not two patients are the same, and settings that optimize ventilation for one patient is unlikely to do the same for other patients.”
Practically, individualized ventilation means continuously adapting ventilation settings to the individual patient. Ventilation can be individualized in different ways, with different tools. It starts with monitoring the patient. Then the doctor or nurse can evaluate the waveforms and adapt e.g., tidal volume and driving pressure accordingly. Studies suggest that performing individualized, lung-protective ventilation includes carefully setting parameters such as tidal volume, plateau pressure, driving pressure, positive end-expiratory pressure, and respiratory rate, to reduce mechanical power delivered to the respiratory system.
Overall, we believe there are three main, direct benefits from individualized ventilation: Synchronization, automation, and consequently a better patient outcome.
“Synchronization and continuous, automatic adjustments of ventilator settings help maintain safe, lung-protective ventilation. This can ultimately improve the treatment and create a better patient outcome”, Tina explains.
Synchronization
Synchronization means patient and ventilator are aligned when it comes to inspiration and expiration, i.e., the ventilator follows the patient’s breathing. When performing respiratory care, it is the goal to have patient and ventilator working in sync. When patient and ventilator are in sync, it is easier for the patient to breathe. Standard settings may be more asynchronous, and thus make it harder for the patient to breathe and result in complications. When the device follows the patient’s breathing synchronously, it is more natural and comfortable for the patient, and it reduces the risk of long-term complications such as VILI.
Automation
Individualized ventilation can be performed automatically with some ventilators. This is carried out by setting targets suited to the individual patient and their current condition. When individualized ventilation is handled automatically, the ventilator can adjust whenever adjustment is needed. This means adjustments are not only made when a nurse or doctor makes a routine check on the patient. In short, automatic adjustments mean less intervention from staff. With constant monitoring from the ventilator, the physical presence of staff is not required all the time, and therefore the patient can be isolated while still cared for. This is a great timesaver for personnel.
Better patient outcome
When using individualized ventilation, patients may suffer fewer injuries from ventilation. In addition to avoiding discomfort, this shortens the hospital stay, which altogether greatly benefits patients. An optimal patient outcome is the overarching goal in healthcare. In this case, shortening the hospital stay also helps to reduce costs.
Individualized ventilation is not a new concept, so what might be preventing staff from using this practice in their everyday? We experience three common obstacles when talking to healthcare personnel.
One potential obstacle is lack of knowledge: Some may not be aware of the potential and benefits of individualized ventilation, as they may not have been exposed to education, studies, and guidelines on the practice.
Another obstacle that is very common when getting started with new ways of working is time: Some staff and departments might have the knowledge and good intentions of getting started but find it hard to allocate the time and resources needed to get a new practice implemented.
The third potential obstacle is resistance to change: Even when you have the knowledge and the time, it might be challenging to implement the new practice, as people often resist change. Therefore, to get new devices and new ways of working implemented successfully and adopted by staff, it requires an active effort.
Knowing the above, it becomes evident that training, support, and time is required to successfully get started with individualized ventilation and get comfortable using it.
There are a variety of ways of getting started with new practices and new devices. Whether lectures, online courses – or a combination – are best for you, depends on your team and work processes.
A plan for successful implementation is crucial. Also, continuously maintaining knowledge on how to perform individualized ventilation is crucial. But first, of course, you need a ventilator.
There are a variety of ventilators available on the market. Some are built for specific uses, e.g., adult or neonatal ventilation, non-invasive ventilation (NIV) or transportation of ventilated patients. Medidyne is a distributor of Hamilton Medical’s ventilators. Hamilton ventilators are known for their innovative features that enable automated, individualized ventilation.
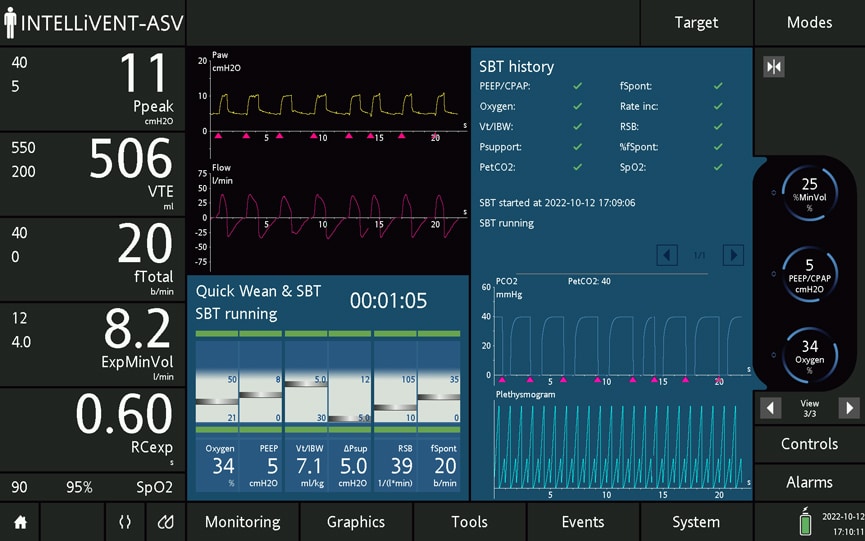
The Hamilton ventilators have the option of utilizing INTELLiVENT-Adaptive Support Ventilation (INTELLiVENT-ASV): A technology built by Hamilton that automatically adjusts ventilation settings to the individual patient’s activity. The effectiveness of the technology has been confirmed in studies: A study of ASV and lung-protective ventilation in ARDS found that settings targeted by ASV were consistent with lung-protective ventilation strategies in ARDS patients both in regards of low tidal volume, driving pressure and mechanical power. Another study of INTELLiVENT-ASV in ICU patients found that INTELLiVENT-ASV is an effective and safe mode of ventilation.
Tina tells: “Hamilton offers a wide range of flexible ventilators for all types of patients and clinical scenarios. The technology and functionality are continuously developed by Hamilton to follow the developments in clinical practices and maintain a high quality.”
If you would like to learn how Hamilton’s ventilators and their innovative technology can support you in your work, feel free to reach out to us for a presentation.
Ventilation that is adapted and continually adjusted to the individual patient helps prevent long-term complications like VILI. It is more comfortable for the patient and may help reduce the length of the hospital stay for the patient. For staff, patient safety and comfort are always at the center, but a shorter hospital stay also equals reduced costs. With ventilators that employ automation, staff can both save time and provide more timely, comfortable, and effective respiratory care for patients.
Er du interesseret i at høre mere så tøv ikke med at tage fat i os – vores dedikerede produktspecialister er kun en e-mail eller et telefonopkald væk.
Area Manager
AccuVein, Avanos Medical, Hamilton Medical, IRadimed, SINAPI Biomedical, Timpel Medical, ZOLL IVTM